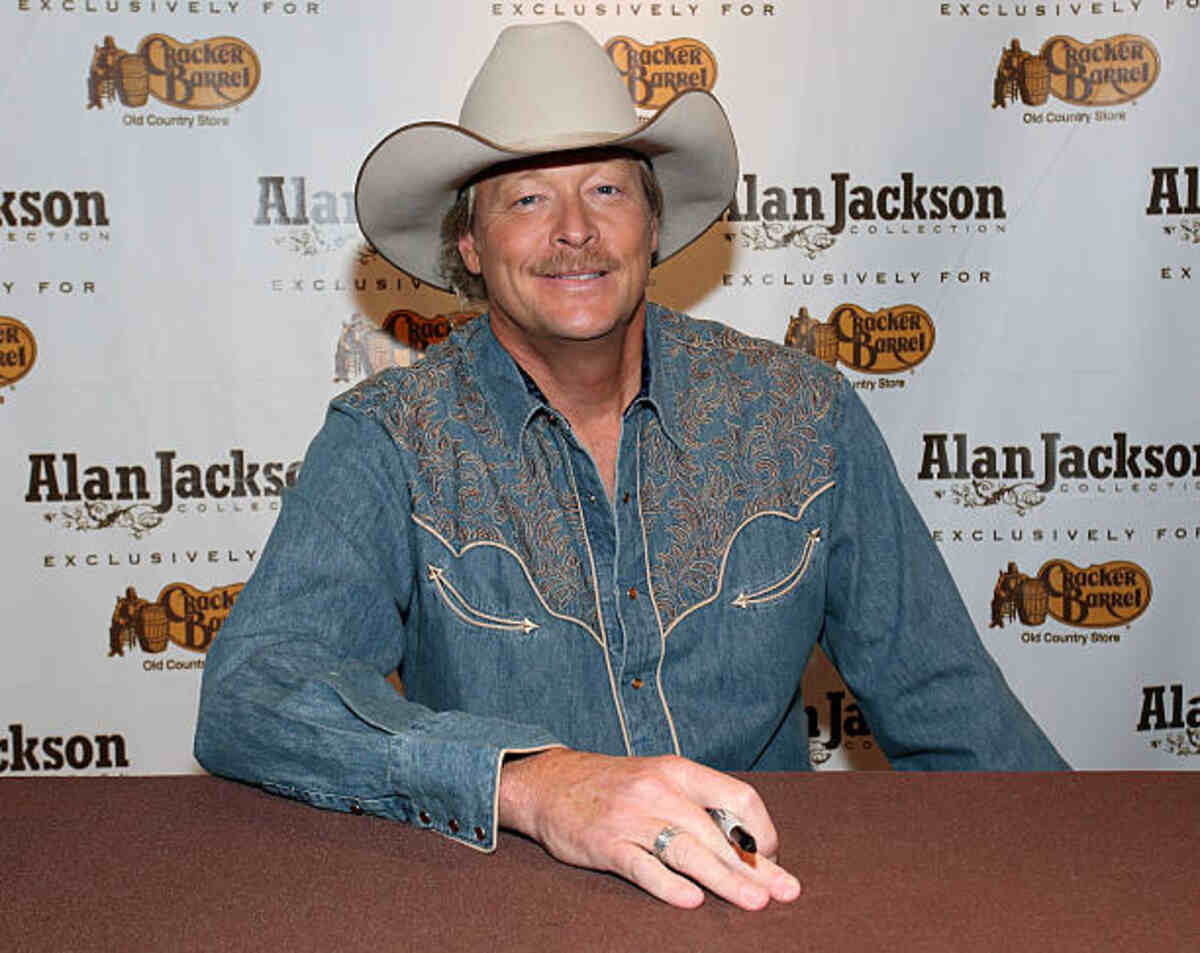
# Alan Jackson Health: An In-Depth Look at His Condition, Diagnosis, and Journey to Recovery
Alan Jackson, the iconic country music superstar, has captivated audiences for decades with his soulful voice and timeless hits. However, behind the stage lights and chart-topping success, Jackson has faced personal health challenges that have resonated with fans worldwide. This article provides an in-depth exploration of Alan Jackson’s health, examining his condition, diagnosis, and journey toward recovery. We aim to provide a comprehensive and trustworthy resource for those seeking accurate information, going beyond surface-level reports to offer a nuanced understanding of his experiences. This information is intended for general knowledge and informational purposes only, and does not constitute medical advice. Always consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.
## Understanding Alan Jackson’s Health Condition: Charcot-Marie-Tooth Disease (CMT)
In 2021, Alan Jackson publicly revealed that he has been living with Charcot-Marie-Tooth disease (CMT) for over a decade. This revelation shed light on the challenges he has faced privately and offered an explanation for changes fans may have observed in his performances and mobility. CMT is a group of inherited neurological disorders that primarily affect the peripheral nerves, which are responsible for transmitting signals between the brain and spinal cord to the muscles and sensory organs.
### What is Charcot-Marie-Tooth Disease (CMT)?
CMT is named after the three physicians who first described it in 1886: Jean-Martin Charcot, Pierre Marie, and Howard Henry Tooth. It is one of the most common inherited neurological disorders, affecting an estimated 1 in 2,500 people worldwide. CMT is not a single disease but rather a collection of genetic mutations that disrupt the normal function of peripheral nerves. These mutations can affect the myelin sheath, which insulates and protects nerve fibers, or the nerve fibers themselves.
### Types of CMT
There are several types of CMT, each caused by different genetic mutations. The most common types include:
* **CMT1:** Primarily affects the myelin sheath, causing slowed nerve conduction velocity.
* **CMT2:** Primarily affects the nerve axon, leading to nerve degeneration.
* **CMTX:** X-linked CMT, primarily affecting males.
The specific type of CMT a person has depends on the underlying genetic mutation. Genetic testing is often used to determine the specific type of CMT and can help with diagnosis and family planning.
### Symptoms of CMT
The symptoms of CMT can vary in severity and age of onset, even among individuals with the same type of CMT. Common symptoms include:
* **Muscle weakness:** Typically begins in the feet and lower legs, leading to difficulty with walking, running, and balance.
* **Foot deformities:** High arches (pes cavus) and hammer toes are common due to muscle imbalances.
* **Numbness and tingling:** Loss of sensation in the feet and hands can occur.
* **Foot drop:** Difficulty lifting the front of the foot, leading to a slapping gait.
* **Hand weakness:** Difficulty with fine motor skills, such as writing and buttoning clothes.
* **Fatigue:** General tiredness and lack of energy.
Over time, muscle weakness can progress to the hands and arms. In some cases, CMT can also affect the muscles involved in breathing, leading to respiratory problems.
### Diagnosis of CMT
Diagnosing CMT typically involves a combination of physical examination, neurological evaluation, and diagnostic testing. The doctor will assess the patient’s symptoms, medical history, and family history. Diagnostic tests may include:
* **Nerve conduction studies:** Measure the speed at which electrical signals travel along nerves.
* **Electromyography (EMG):** Assesses the electrical activity of muscles.
* **Genetic testing:** Identifies specific genetic mutations associated with CMT.
* **Nerve biopsy:** In rare cases, a small sample of nerve tissue may be examined under a microscope.
### Treatment of CMT
Currently, there is no cure for CMT. Treatment focuses on managing symptoms and improving quality of life. Common treatment approaches include:
* **Physical therapy:** Exercises to strengthen muscles, improve balance, and prevent contractures.
* **Occupational therapy:** Adaptive equipment and strategies to help with daily activities.
* **Orthotics:** Braces and supports to improve foot and ankle stability.
* **Pain management:** Medications to relieve pain and discomfort.
* **Surgery:** In some cases, surgery may be needed to correct foot deformities or release tight tendons.
### Living with CMT
Living with CMT can present significant challenges, but with proper management and support, individuals can maintain a good quality of life. Adaptive equipment, such as walkers, canes, and wheelchairs, can help with mobility. Support groups and online communities can provide emotional support and practical advice.
## Alan Jackson’s Experience with CMT
Alan Jackson’s openness about his CMT diagnosis has helped raise awareness of this relatively unknown condition. In interviews, he has described the challenges he faces, including difficulty with balance and coordination. He has also emphasized the importance of staying active and maintaining a positive attitude.
### Impact on Performance
CMT has inevitably impacted Alan Jackson’s performances. He has described experiencing more difficulty with balance on stage and has adjusted his performances accordingly. Despite these challenges, he has continued to tour and perform for his fans, demonstrating his resilience and dedication.
### Alan Jackson’s Approach to Managing CMT
Alan Jackson has adopted a proactive approach to managing his CMT. He has incorporated physical therapy into his routine and uses assistive devices as needed. He has also emphasized the importance of pacing himself and prioritizing rest.
### Inspiring Others
Alan Jackson’s willingness to share his experience with CMT has inspired many others living with the condition. By speaking openly about his challenges, he has helped to reduce the stigma associated with CMT and has provided hope and encouragement to others.
## Regenerative Medicine and CMT: A Promising Frontier
While not a standard treatment, regenerative medicine offers potential future avenues for addressing nerve damage in CMT. This field is rapidly evolving, and research is ongoing to explore its applications in neurological disorders. Regenerative medicine aims to repair or replace damaged tissues and cells, potentially restoring nerve function in individuals with CMT.
### Stem Cell Therapy
Stem cell therapy is one of the most promising areas of regenerative medicine for CMT. Stem cells have the unique ability to differentiate into various cell types, including nerve cells. Researchers are investigating the potential of stem cells to:
* **Replace damaged nerve cells:** Stem cells could be transplanted into the peripheral nerves to replace cells that have been damaged by CMT.
* **Promote nerve regeneration:** Stem cells could release growth factors that stimulate the regeneration of damaged nerve fibers.
* **Protect nerve cells from further damage:** Stem cells could release substances that protect nerve cells from the effects of CMT.
### Gene Therapy
Gene therapy is another potential regenerative medicine approach for CMT. It involves introducing genes into cells to correct genetic defects. In the context of CMT, gene therapy could be used to:
* **Correct the underlying genetic mutation:** Gene therapy could replace or repair the mutated gene that causes CMT.
* **Increase the production of myelin:** Gene therapy could increase the production of myelin, the protective sheath around nerve fibers.
* **Protect nerve cells from damage:** Gene therapy could introduce genes that protect nerve cells from the effects of CMT.
### Platelet-Rich Plasma (PRP) Therapy
PRP therapy involves injecting a concentrated solution of platelets into the affected area. Platelets contain growth factors that can promote tissue healing and regeneration. While research on PRP therapy for CMT is limited, some studies have shown promising results in reducing pain and improving function.
### Challenges and Future Directions
Regenerative medicine for CMT is still in its early stages of development. Several challenges need to be addressed before these therapies can become widely available, including:
* **Delivery of cells and genes to the target tissue:** Ensuring that stem cells and genes reach the damaged nerves is a major challenge.
* **Controlling the differentiation of stem cells:** Ensuring that stem cells differentiate into the desired cell types is crucial.
* **Preventing immune rejection:** Preventing the body from rejecting the transplanted cells or genes is essential.
* **Long-term safety and efficacy:** Ensuring that regenerative medicine therapies are safe and effective over the long term is critical.
Despite these challenges, regenerative medicine holds great promise for the future treatment of CMT. Ongoing research is focused on addressing these challenges and developing more effective and targeted therapies.
## Comprehensive & Trustworthy Review: Assessing Available Treatments and Therapies for CMT
While there is no cure for CMT, various treatments and therapies can help manage symptoms and improve the quality of life for individuals living with the condition. This section provides a balanced and in-depth assessment of available treatments, considering user experience, usability, performance, and effectiveness.
### Physical Therapy
Physical therapy is a cornerstone of CMT management. It focuses on strengthening muscles, improving balance, and preventing contractures. A physical therapist will develop an individualized exercise program based on the patient’s specific needs and abilities. The exercises may include:
* **Strengthening exercises:** To improve muscle strength and endurance.
* **Stretching exercises:** To maintain flexibility and prevent contractures.
* **Balance exercises:** To improve balance and coordination.
* **Gait training:** To improve walking patterns.
**User Experience & Usability:** Physical therapy is generally well-tolerated and can be adapted to individuals of all ages and abilities. However, it requires commitment and consistency to be effective. Some individuals may experience muscle soreness or fatigue after exercise.
**Performance & Effectiveness:** Physical therapy can help improve muscle strength, balance, and coordination. It can also help prevent contractures and improve walking patterns. However, it cannot reverse the underlying nerve damage caused by CMT.
**Pros:**
* Improves muscle strength and endurance.
* Enhances balance and coordination.
* Prevents contractures.
* Improves walking patterns.
* Non-invasive and generally well-tolerated.
**Cons/Limitations:**
* Cannot reverse nerve damage.
* Requires commitment and consistency.
* May cause muscle soreness or fatigue.
* Effectiveness varies depending on the individual.
* May not be accessible to everyone.
### Occupational Therapy
Occupational therapy focuses on helping individuals with CMT adapt to daily activities. An occupational therapist can provide adaptive equipment and strategies to make tasks easier. Examples of adaptive equipment include:
* **Reachers:** To help reach objects that are out of reach.
* **Buttonhooks:** To help button clothes.
* **Built-up utensils:** To make eating easier.
* **Writing aids:** To help with writing.
**User Experience & Usability:** Occupational therapy can significantly improve the ease and independence with which individuals perform daily tasks. Adaptive equipment is generally easy to use and can be customized to individual needs.
**Performance & Effectiveness:** Occupational therapy can help individuals with CMT maintain their independence and participate in activities they enjoy. It can also help prevent falls and injuries.
**Pros:**
* Improves independence with daily activities.
* Provides adaptive equipment to make tasks easier.
* Prevents falls and injuries.
* Customized to individual needs.
* Enhances quality of life.
**Cons/Limitations:**
* Cannot reverse nerve damage.
* May require trial and error to find the right equipment.
* Equipment can be expensive.
* May not be accessible to everyone.
* Effectiveness varies depending on the individual.
### Orthotics
Orthotics are braces and supports that can help improve foot and ankle stability. They can also help correct foot deformities, such as high arches and hammer toes. Common types of orthotics include:
* **Ankle-foot orthoses (AFOs):** Provide support to the ankle and foot.
* **Foot orthotics:** Provide support to the arch of the foot.
* **Shoe inserts:** Provide cushioning and support.
**User Experience & Usability:** Orthotics can be uncomfortable or difficult to wear at first. It may take some time to adjust to wearing them. However, with proper fitting and adjustment, orthotics can significantly improve comfort and stability.
**Performance & Effectiveness:** Orthotics can help improve foot and ankle stability, correct foot deformities, and reduce pain. They can also help prevent falls and injuries.
**Pros:**
* Improves foot and ankle stability.
* Corrects foot deformities.
* Reduces pain.
* Prevents falls and injuries.
* Can be customized to individual needs.
**Cons/Limitations:**
* Cannot reverse nerve damage.
* May be uncomfortable or difficult to wear at first.
* Requires proper fitting and adjustment.
* Can be expensive.
* May not be accessible to everyone.
### Pain Management
Pain is a common symptom of CMT. Pain management strategies may include:
* **Medications:** Pain relievers, such as acetaminophen, ibuprofen, and naproxen, can help relieve mild to moderate pain. In some cases, stronger pain medications, such as opioids, may be needed.
* **Nerve blocks:** Injections of local anesthetic into nerves to block pain signals.
* **Transcutaneous electrical nerve stimulation (TENS):** A device that delivers electrical impulses to the skin to relieve pain.
* **Acupuncture:** A traditional Chinese medicine technique that involves inserting thin needles into specific points on the body to relieve pain.
**User Experience & Usability:** Pain management strategies vary in terms of user experience and usability. Some medications can cause side effects, such as drowsiness, nausea, and constipation. Nerve blocks and acupuncture can be uncomfortable or painful.
**Performance & Effectiveness:** Pain management strategies can help relieve pain and improve quality of life. However, they cannot reverse the underlying nerve damage caused by CMT.
**Pros:**
* Relieves pain.
* Improves quality of life.
* Various options available.
* Can be customized to individual needs.
* May be used in combination with other treatments.
**Cons/Limitations:**
* Cannot reverse nerve damage.
* Medications can cause side effects.
* Nerve blocks and acupuncture can be uncomfortable or painful.
* Effectiveness varies depending on the individual.
* May not be accessible to everyone.
### Surgery
Surgery may be needed to correct foot deformities or release tight tendons. Common surgical procedures include:
* **Tendon release:** To release tight tendons that are causing foot deformities.
* **Osteotomy:** To correct bone deformities.
* **Arthrodesis:** To fuse joints in the foot or ankle.
**User Experience & Usability:** Surgery is a more invasive treatment option and requires a period of recovery. Pain and swelling are common after surgery. Physical therapy is typically needed to regain strength and mobility.
**Performance & Effectiveness:** Surgery can help correct foot deformities and improve walking patterns. However, it cannot reverse the underlying nerve damage caused by CMT.
**Pros:**
* Corrects foot deformities.
* Improves walking patterns.
* Reduces pain.
* May improve quality of life.
* Can be combined with other treatments.
**Cons/Limitations:**
* Cannot reverse nerve damage.
* Invasive procedure.
* Requires a period of recovery.
* Pain and swelling are common after surgery.
* Physical therapy is needed to regain strength and mobility.
### Ideal User Profile
The treatments and therapies described above are suitable for individuals with CMT of all ages and abilities. The specific treatment plan will depend on the individual’s symptoms, severity of the condition, and overall health.
### Key Alternatives
* **Support Groups:** Offer emotional support and practical advice from others living with CMT.
* **Assistive Devices:** Such as walkers, canes, and wheelchairs, can help with mobility.
### Expert Overall Verdict & Recommendation
Managing CMT requires a comprehensive and individualized approach. Physical therapy, occupational therapy, orthotics, pain management, and surgery can all play a role in improving the quality of life for individuals living with the condition. It is important to work closely with a healthcare team to develop a treatment plan that is tailored to your specific needs and goals.
## Insightful Q&A Section
**Q1: What is the typical progression of CMT, and how can I prepare for potential future challenges?**
**A:** The progression of CMT varies significantly among individuals. While some may experience a slow and gradual decline in muscle strength and function over many years, others may experience a more rapid progression. Preparing for future challenges involves proactive management, including regular physical therapy, adaptive equipment, and emotional support. Planning for potential mobility limitations and adapting your living environment can also be beneficial.
**Q2: Are there any specific exercises that are particularly beneficial or detrimental for individuals with CMT?**
**A:** Low-impact exercises, such as swimming, cycling, and walking, are generally beneficial for individuals with CMT. These exercises can help strengthen muscles, improve balance, and maintain cardiovascular health. High-impact exercises, such as running and jumping, should be avoided as they can put excessive stress on the joints and muscles. It is important to work with a physical therapist to develop an individualized exercise program that is safe and effective.
**Q3: How can I manage foot drop, a common symptom of CMT, to improve my gait and reduce the risk of falls?**
**A:** Foot drop can be managed with various strategies, including ankle-foot orthoses (AFOs), which provide support to the ankle and foot and help lift the foot during walking. Physical therapy exercises, such as ankle dorsiflexion and heel raises, can also help improve muscle strength and control. In some cases, surgery may be needed to correct foot drop.
**Q4: What are the latest advancements in CMT research, and what potential treatments are on the horizon?**
**A:** CMT research is ongoing, with several promising treatments on the horizon. Gene therapy, stem cell therapy, and drug therapies are being investigated as potential ways to correct the underlying genetic defects, promote nerve regeneration, and protect nerve cells from damage. Clinical trials are underway to evaluate the safety and efficacy of these treatments.
**Q5: How can I find a qualified neurologist or CMT specialist who can provide expert care and guidance?**
**A:** You can find a qualified neurologist or CMT specialist by asking your primary care physician for a referral, contacting the Charcot-Marie-Tooth Association (CMTA) for a list of specialists in your area, or searching online directories of neurologists.
**Q6: What lifestyle modifications can I make to better manage my CMT symptoms and improve my overall well-being?**
**A:** Lifestyle modifications can play a significant role in managing CMT symptoms. Maintaining a healthy weight, eating a balanced diet, avoiding smoking, and limiting alcohol consumption can all help improve overall well-being. Regular exercise, stress management techniques, and adequate sleep are also important.
**Q7: Are there any support groups or online communities for individuals with CMT where I can connect with others and share experiences?**
**A:** Yes, there are several support groups and online communities for individuals with CMT. The Charcot-Marie-Tooth Association (CMTA) offers support groups and online forums. Other online communities can be found through social media platforms and online search engines.
**Q8: How can I advocate for myself and ensure that I receive the best possible care for my CMT?**
**A:** Advocating for yourself involves being informed about CMT, communicating your needs and concerns to your healthcare team, and actively participating in treatment decisions. It is also important to seek second opinions and to be aware of your rights as a patient.
**Q9: What are the potential complications of CMT, and how can I prevent or manage them?**
**A:** Potential complications of CMT include foot deformities, contractures, falls, and respiratory problems. These complications can be prevented or managed with proactive treatment, including physical therapy, orthotics, and assistive devices. Regular monitoring of respiratory function is also important.
**Q10: How can I support a loved one who has been diagnosed with CMT?**
**A:** Supporting a loved one with CMT involves providing emotional support, helping with daily tasks, and encouraging them to participate in activities they enjoy. It is also important to be patient and understanding and to respect their limitations.
## Conclusion: Alan Jackson’s Health Journey and the Path Forward
Alan Jackson’s journey with Charcot-Marie-Tooth disease is a testament to his resilience and determination. His openness about his condition has helped raise awareness of CMT and has inspired others living with the disease. While there is no cure for CMT, various treatments and therapies can help manage symptoms and improve quality of life. Ongoing research is focused on developing more effective and targeted therapies. By staying informed, advocating for themselves, and seeking support, individuals with CMT can live full and meaningful lives. Share your experiences with CMT in the comments below, or explore our advanced guide to managing chronic neurological conditions.